Sixteen milliseconds - one-fifth the speed of the blink of an eye - can mean the difference between life and death for millions of people. How can such a miniscule amount of time have such a profound effect on so many? That's about how long it takes for one infinitesimal cancer cell to adhere to a new location within the body. In as little as a day, a new tumor is born in a phenomenon known as metastasizing.
The American Cancer Society forecasts that nearly 1.5 million new cases of cancer will be diagnosed this year alone, and for many patients, fear of metastasis will dominate their treatment. It takes just one cell, measuring about one-fourth the width of a human hair, to begin a new tumor in a secondary site. Often renegade cells travel through the lymphatic system, where they might get caught up in lymph nodes near the primary site. Other times, they travel through the blood stream, where they can make their way to any location within the body.
Exactly what causes cancer cells to break away and travel remains a challenge for cancer researchers, but scientists at The Pennsylvania State University (PSU) are zeroing in on how cells adhere in the new location, and what might be done to influence this adhesion. To do so, they are employing pioneering computational fluid dynamics simulations made possible by Harpoon 3D mesh generator from Sharc Ltd. in the UK, and EnSight extreme visualization software by CEI, Inc. of Apex, NC.
Meghan Hoskins, a Ph.D. candidate in the Bioengineering program at Penn State, under the advisement of Robert Kunz, Ph.D. and Cheng Dong, Ph.D., is examining how cancer cells stick to white blood cells, the defenders of the blood stream, and how the flow of blood affects this adhesion. Her work, funded by the National Cancer Institute and the PSU Applied Research Laboratory, is based on the theory that, as cancer cells travel through the blood stream, they are attracted to areas where white blood cells are at work fighting inflammation.
“If there is already inflammation in the body, that could actually attract the cancer cells,” Hoskins says, noting that the patient may be totally unaware of the inflammation. “Cancer cells are also capable of secreting certain proteins that can activate the white blood cells, so there's a possibility that cancer cells can themselves create a localized inflammation, even if there isn't one there to begin with.”
This frightening concept, that cancer cells can actually use our own immune system against us, is the foundation of Hoskins research. Her goal is to accurately simulate previous experimental conditions of this phenomenon to validate her model, so that it may be used to further study the metastasis process. To do so, Hoskins is developing a simulated system, based on an existing rectangular test chamber in Professor Dong's lab, designed to study the flow of these proteins to the white blood cells and how this affects the adhesion.
Existing experimental data suggests that shear rate, the change in flow velocity within the micro capillaries, can affect the adhesion of tumor cells. By devising computational fluid dynamics models of the chamber, Hoskins is calculating velocity profiles throughout the test chamber and attempting to characterize the dynamic forces and biochemistry at work during in vitro cell adhesion.
To develop the model, Hoskins is using Harpoon, a fully automatic extreme mesh generator, to construct a detailed 3D geometric grid of the experimental flow chamber. At each time step, which ranges from 1 to 8 microseconds, Hoskins performs a quasi-steady CFD calculation to ascertain the fluid forces on the tumor cells. She then generates a new Harpoon grid.
“Harpoon has been pretty important in my work because I'm doing such small time steps with so much going on simultaneously,” Hoskins says. “I need something that can work quickly, and Harpoon has been very fast. Each time I make a new grid, it takes less than 30 seconds. Without Harpoon, I would have to generate each grid by hand, which could take hours, depending on the complexity of the grid.”
The results are exported to the AcuSolve flow solver for CFD analysis. Motion is then calculated by solving the six-degrees-of-freedom (6DOF) dynamics system for the cells in a Python script. This calculation allows Hoskins to determine exactly where and how fast the cells move at each step within the three-dimensional field.
Each simulation took approximately 2000 time steps with Harpoon running at each iteration. When a cell is deformable, Harpoon runs twice for each time step, so 4000 times per simulation. Hoskins estimates that she has run Harpoon approximately 60,000 times. Meshing this by hand would have taken over 21 years, using Harpoon it only took 21 days!
So far, Hoskins plans to model two experimental setups. The first is called a migration chamber - a rectangular flow chamber with holes in the bottom surface on which a filter is placed that allows cells to migrate through it. Endothelium cells, like those that form the inside lining of the blood vessels, are cultured on top of the filter. A solution of white blood cells and cancer cells are perfused through the inside. In this model, when only cancer cells are present in the chamber, there is significantly less migration of those cells through the endothelium than when white blood cells are also present. This suggests that the white blood cells influence the migration.
In the second model, the chamber is sealed. Researchers can watch as the cells interact, collide and adhere to one another, and measure how much of this activity takes place. In this instance, it has been found that shear rate, or velocity, affects the cancer cell's adhesion to white blood cells. But, the adhesion of white blood cells to the endothelial cells is affected by both shear rate and shear stress, or the force produced by the flow.
Hoskins' mission is to understand why and how the migration of cancer cells is affected by the fluid dynamics of the system. This knowledge could help determine targets for future therapeutic research. For example, if she can identify that cancer-produced proteins carried through the blood stream do significantly activate the white blood cells, perhaps medical researchers can devise a way to block the activity of those proteins.
For right now, though, Hoskins' is laying the groundwork for future research by providing insight into the adhesion process. She continues to make improvements to the model to more accurately simulate in vivo metastasis.
“In early models, for simplicity, I kept the cells rigid. But, in reality both the cancer cell and white blood cells are flexible. I'm working on a new model that allows the cells to deform. Both the flow and the collision between the two affects the shape of the cells,” Hoskins says. “This could change how the adhesion takes place. If the cells can deform, there might be a larger area for adhesion bonds to form.”
For future study, Hoskins hopes that her model will see continued improvement, particularly with regard to simulating adhesion within the geometry of actual blood vessel shapes. Once her model is validated, the options for future study are open to many possibilities. For the 10.5 million people now living with a history of cancer in the United States alone, this offers a glimmer of hope that some day future generations will not have to live in fear of metastasizing cancer.

One deformable cancer cell traverses the white blood cell in this EnSight image.
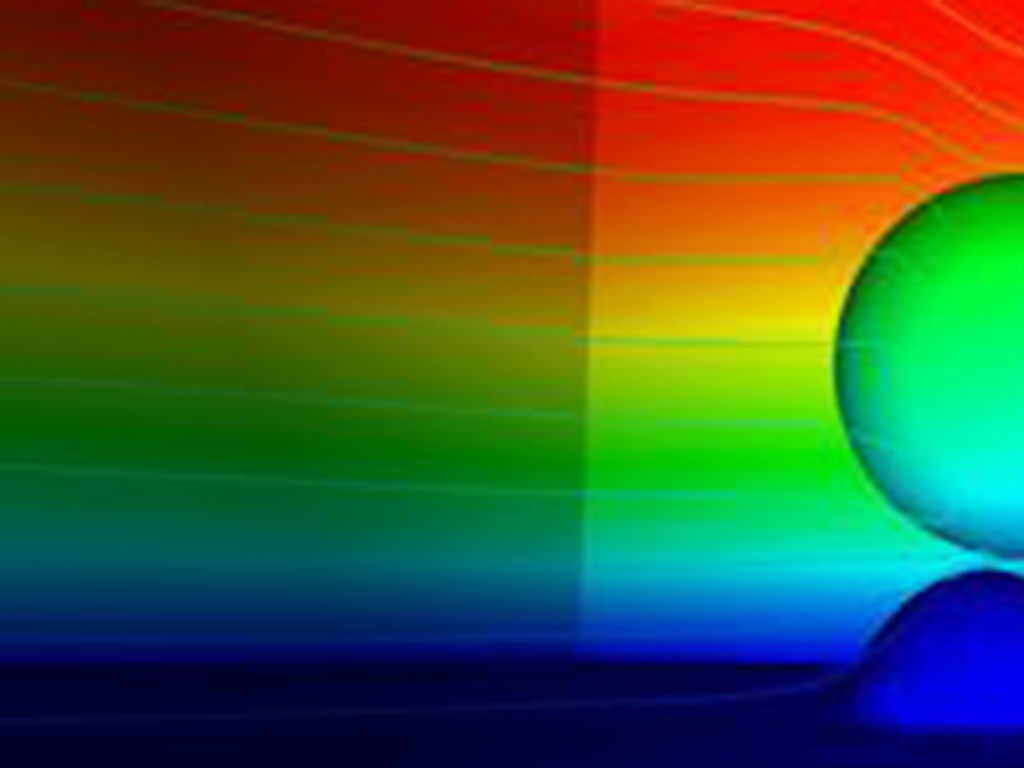
A cancer cell flows over the white blood cell without any bond interactions or deformation.